That seemingly innocent bottle of ibuprofen in your medicine cabinet might be doing more than just relieving your headache—it could be interfering with your blood pressure medication in ways you never imagined. While over-the-counter (OTC) medications offer convenient relief for everyday ailments, they're far from harmless when combined with prescription drugs.
If you're managing multiple health conditions with prescription medications, understanding these interactions becomes crucial for your safety and well-being. The reality is that many adults unknowingly create dangerous combinations by mixing their prescribed treatments with readily available OTC products. But here's the empowering news: with the right knowledge and simple precautions, you can safely navigate both worlds.
Let's explore the most common OTC culprits that could be affecting your prescriptions and discover practical strategies to keep your medication routine both effective and safe.
NSAIDs: The Hidden Troublemakers in Your Medicine Cabinet
Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin), naproxen (Aleve), and aspirin are among the most commonly used OTC medications. They're incredibly effective for pain relief and reducing inflammation, but they can create serious complications when combined with certain prescriptions.
Blood Pressure Medications at Risk
If you're taking ACE inhibitors (like lisinopril) or diuretics (water pills) for blood pressure control, NSAIDs can significantly reduce their effectiveness. These pain relievers can cause your body to retain sodium and water, directly counteracting the blood pressure-lowering effects of your prescriptions.
This interaction is particularly concerning because it's often invisible—you won't feel the reduced effectiveness until your blood pressure readings show the problem. Studies reveal that regular NSAID use can increase blood pressure by 5-10 mmHg, potentially negating months of successful treatment.
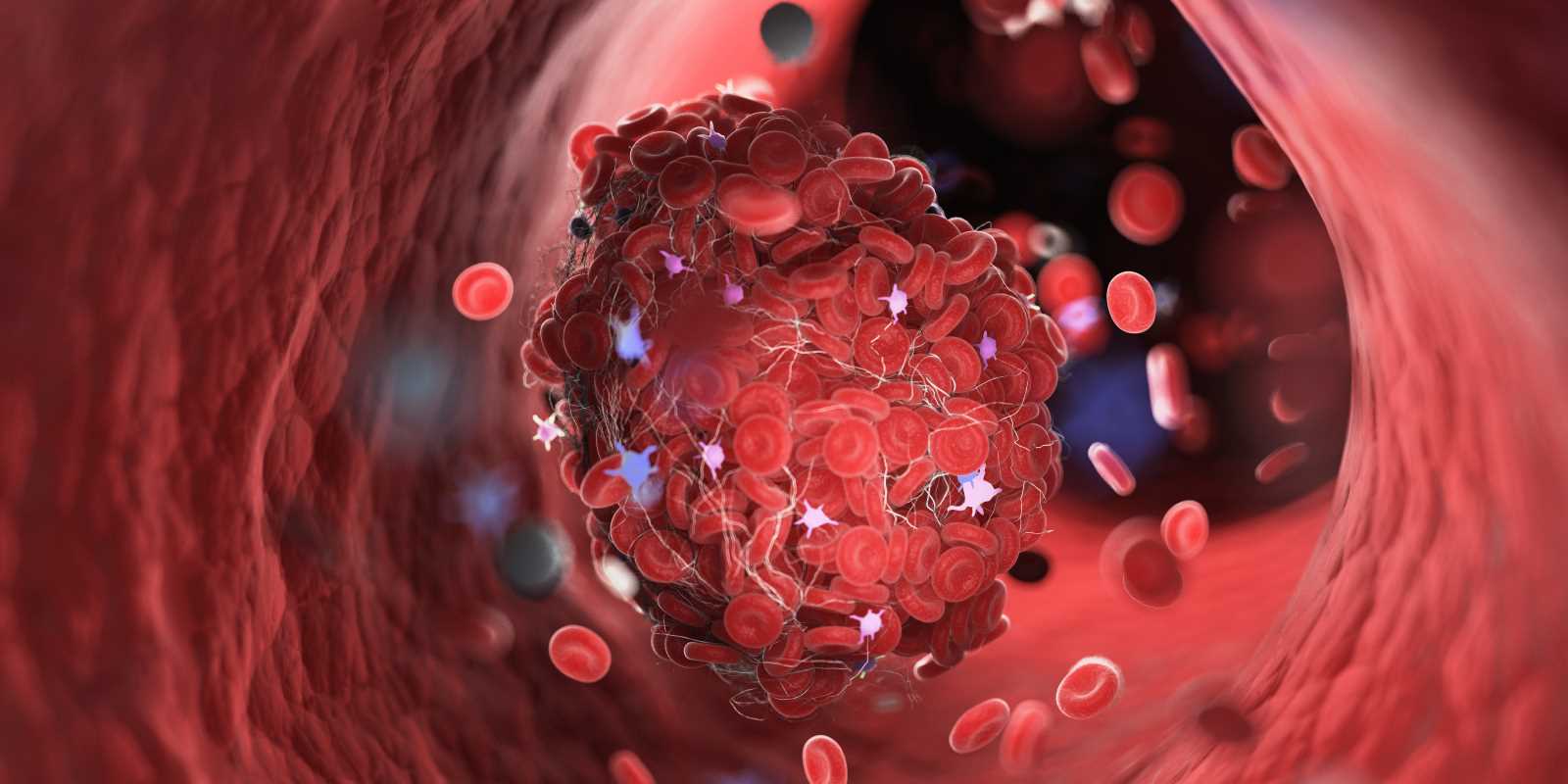
Blood Thinners and Bleeding Risks
The combination of NSAIDs with blood thinners like warfarin (Coumadin) or newer anticoagulants creates a perfect storm for bleeding complications. Both drug types affect your blood's ability to clot, and when combined, they can dramatically increase bleeding risk.
Even seemingly minor injuries like cuts or bruises can become serious when these medications interact. Internal bleeding, particularly in the stomach, becomes a genuine concern that could require emergency medical attention.
Safer alternatives: If you need pain relief while taking blood pressure medications or blood thinners, acetaminophen (Tylenol) is generally a safer choice. Always consult your healthcare provider before making switches, as individual circumstances vary.
Antacids: More Than Stomach Relief
Those chalky tablets that provide quick heartburn relief can significantly impact how your body absorbs prescription medications. Antacids work by neutralizing stomach acid, but many medications require that acidic environment to dissolve and absorb properly.
Thyroid Medications Under Threat
Levothyroxine, the most commonly prescribed thyroid hormone replacement, is particularly vulnerable to antacid interference. The calcium and magnesium in antacids can bind to levothyroxine in your stomach, preventing absorption and leaving you with inadequate hormone levels.
This interaction can leave you feeling fatigued, depressed, and experiencing other symptoms of underactive thyroid function, even while taking your prescribed dose. The timing of this interaction is crucial—taking antacids within four hours of thyroid medication can reduce absorption by up to 40%.
Antibiotic Absorption Issues
Many antibiotics, including quinolones (like ciprofloxacin) and tetracyclines, form complexes with the minerals in antacids. This binding prevents the antibiotic from being absorbed into your bloodstream, potentially allowing infections to persist or worsen.
Iron supplements face similar challenges, with antacids reducing iron absorption by up to 60%. For adults managing anemia or iron deficiency, this interaction can significantly delay recovery and maintain troublesome symptoms like fatigue and weakness.
Smart spacing strategy: Create at least a two-hour buffer between antacids and other medications. Take your prescriptions first, then wait before addressing heartburn symptoms.
Antihistamines: Drowsiness and Beyond
Popular allergy medications like diphenhydramine (Benadryl), loratadine (Claritin), and cetirizine (Zyrtec) seem harmless enough, but they can amplify the sedating effects of other medications in unexpected ways.
Magnifying Sedation Effects
If you're taking medications that cause drowsiness—such as certain antidepressants, anxiety medications, or sleep aids—adding antihistamines can create dangerous levels of sedation. This combination increases fall risk, impairs driving ability, and can cause confusion, particularly in older adults.
The interaction becomes more pronounced with first-generation antihistamines like Benadryl, which cross into the brain more readily than newer formulations. Even during daytime use, this combination can cause unexpected sleepiness and cognitive impairment.
Blood Pressure Complications
Some antihistamines, particularly first-generation types, can interfere with blood pressure medications by affecting your cardiovascular system. They may counteract the effects of beta-blockers or cause irregular heart rhythms in sensitive individuals.
Wiser choices: If you need allergy relief while taking sedating medications, consider second-generation antihistamines like loratadine (Claritin) or cetirizine (Zyrtec), which cause less drowsiness and fewer interactions.
Herbal Supplements: Natural Doesn't Mean Harmless
The supplement aisle offers countless natural remedies, but several popular herbs can significantly interfere with prescription medications. Unlike FDA-regulated drugs, supplements aren't required to provide interaction warnings, making them particularly tricky to navigate safely.
St. John's Wort: The Medication Accelerator
This popular herbal antidepressant is one of the most problematic supplements when it comes to drug interactions. St. John's Wort dramatically increases the activity of liver enzymes responsible for breaking down medications, causing your prescriptions to be metabolized much faster than intended.
This acceleration can render many medications ineffective, including:
- Birth control pills (increasing pregnancy risk)
- Blood thinners like warfarin
- Heart medications like digoxin
- Antidepressants and anxiety medications
- Immunosuppressive drugs
The interaction is so significant that some medications become completely ineffective, potentially creating life-threatening situations for people with serious health conditions.
Ginkgo Biloba and Bleeding Risks
Marketed for memory enhancement, ginkgo biloba can increase bleeding risk when combined with blood-thinning medications. This herb affects platelet function, and when combined with prescription anticoagulants, it can lead to serious bleeding complications.
Garlic Supplements and Blood Sugar
While fresh garlic in cooking is generally safe, concentrated garlic supplements can interact with diabetes medications, potentially causing dangerously low blood sugar levels. This interaction is particularly concerning because hypoglycemia can develop rapidly and without warning.
Research requirement: Before adding any herbal supplement to your routine, research potential interactions with your current medications and discuss them with your healthcare provider or pharmacist.
Vitamin and Mineral Supplements: Surprising Interactions
Even basic vitamins and minerals can interfere with prescription medications in ways that might surprise you.
Calcium's Multiple Interferences
Calcium supplements don't just affect antacids—they can interfere with numerous medications:
- Thyroid hormones (reducing absorption)
- Certain antibiotics (forming complexes that can't be absorbed)
- Bisphosphonates for osteoporosis (dramatically reducing effectiveness)
- Some blood pressure medications
Iron's Complicated Relationships
Iron supplements can reduce the effectiveness of several medications, including certain antibiotics and thyroid hormones. Conversely, some medications can reduce iron absorption, creating a complex web of interactions that requires careful timing.
Vitamin K and Blood Thinners
If you're taking warfarin, sudden increases in vitamin K intake (through supplements or dramatic dietary changes) can reduce the medication's effectiveness. While this doesn't mean avoiding vitamin K entirely, consistency in intake becomes crucial for maintaining stable blood-thinning effects.
Practical Strategies for Safe OTC Use
Successfully managing OTC and prescription medications together requires a proactive approach and clear communication with your healthcare team.
Create a Comprehensive Medication List
Develop a complete inventory that includes everything you take regularly:
- All prescription medications with dosages
- OTC medications you use even occasionally
- Vitamins, minerals, and herbal supplements
- Protein powders or meal replacements that contain added nutrients
Update this list immediately whenever you add or remove anything, and bring it to every medical appointment.
Master the Art of Label Reading
OTC medication labels contain crucial interaction information, but it's often buried in small print. Look specifically for:
- Warnings about use with blood thinners, blood pressure medications, or diabetes drugs
- Instructions about spacing doses from other medications
- Contraindications for specific health conditions you have
Many labels now include QR codes that link to more detailed interaction information—take advantage of this technology for comprehensive safety data.
Build a Partnership with Your Pharmacist
Your pharmacist is an underutilized resource for interaction prevention. They have access to sophisticated screening software that can identify potential problems across all your medications and supplements.
Make your pharmacist your ally by:
- Using the same pharmacy for all prescriptions when possible
- Asking about interactions before purchasing new OTC products
- Requesting printed interaction information for future reference
- Discussing timing strategies for medications that must be spaced apart
Timing Is Everything
Many interactions can be avoided through strategic timing rather than complete avoidance:
- Take prescription medications first, then wait 2-4 hours before OTC products
- Spread doses throughout the day when possible
- Use smartphone reminders to maintain consistent spacing
- Keep a simple timing chart until the routine becomes automatic
When to Seek Professional Guidance
Contact your healthcare provider or pharmacist immediately if you experience:
- New or unusual symptoms after starting an OTC medication
- Changes in how you feel on your regular prescriptions
- Questions about specific combinations you're considering
- Side effects that seem stronger than expected
Don't wait for your next scheduled appointment if you have concerns—most healthcare providers prefer preventing problems rather than treating complications.
Technology Tools for Safer Management
Modern technology offers excellent support for managing medication interactions:
Interaction checking apps: Several free smartphone apps allow you to check interactions before taking new medications. Popular options include drug interaction checkers from reputable medical sources.
Medication management apps: These tools can track all your medications and supplements while sending reminders and interaction alerts.
Pharmacy apps: Many pharmacy chains offer apps that maintain your medication history and can screen for interactions when filling new prescriptions.
Disclaimer: The content provided on SuperHealthyTips is for informational and educational purposes only. This information is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
 (Image via
(Image via.jpg)