Turning 40 marks a crossroad where many people start paying closer attention to their health numbers. During routine check-ups, conversations about cholesterol levels become more frequent, and your doctor might mention statins for the first time. These cholesterol-lowering medications have become one of the most commonly prescribed drugs worldwide, yet the decision to start taking them involves careful consideration of both benefits and potential drawbacks.
Understanding statins becomes particularly important as you navigate your 40s and beyond. Your body's metabolism changes, family history becomes more relevant, and the cumulative effects of lifestyle choices start showing up in blood tests. Making an informed decision about statin therapy requires examining the evidence, weighing personal risk factors, and considering alternative approaches to heart health.
Let's explore the complete picture of statin therapy after 40, helping you approach this important health decision with confidence and clarity.
Understanding Statins and How They Work
Statins belong to a class of medications that block an enzyme your liver uses to produce cholesterol. By reducing cholesterol production, these drugs lower the amount of low-density lipoprotein (LDL) or "bad" cholesterol circulating in your bloodstream. Common statin medications include atorvastatin (Lipitor), simvastatin (Zocor), and rosuvastatin (Crestor).
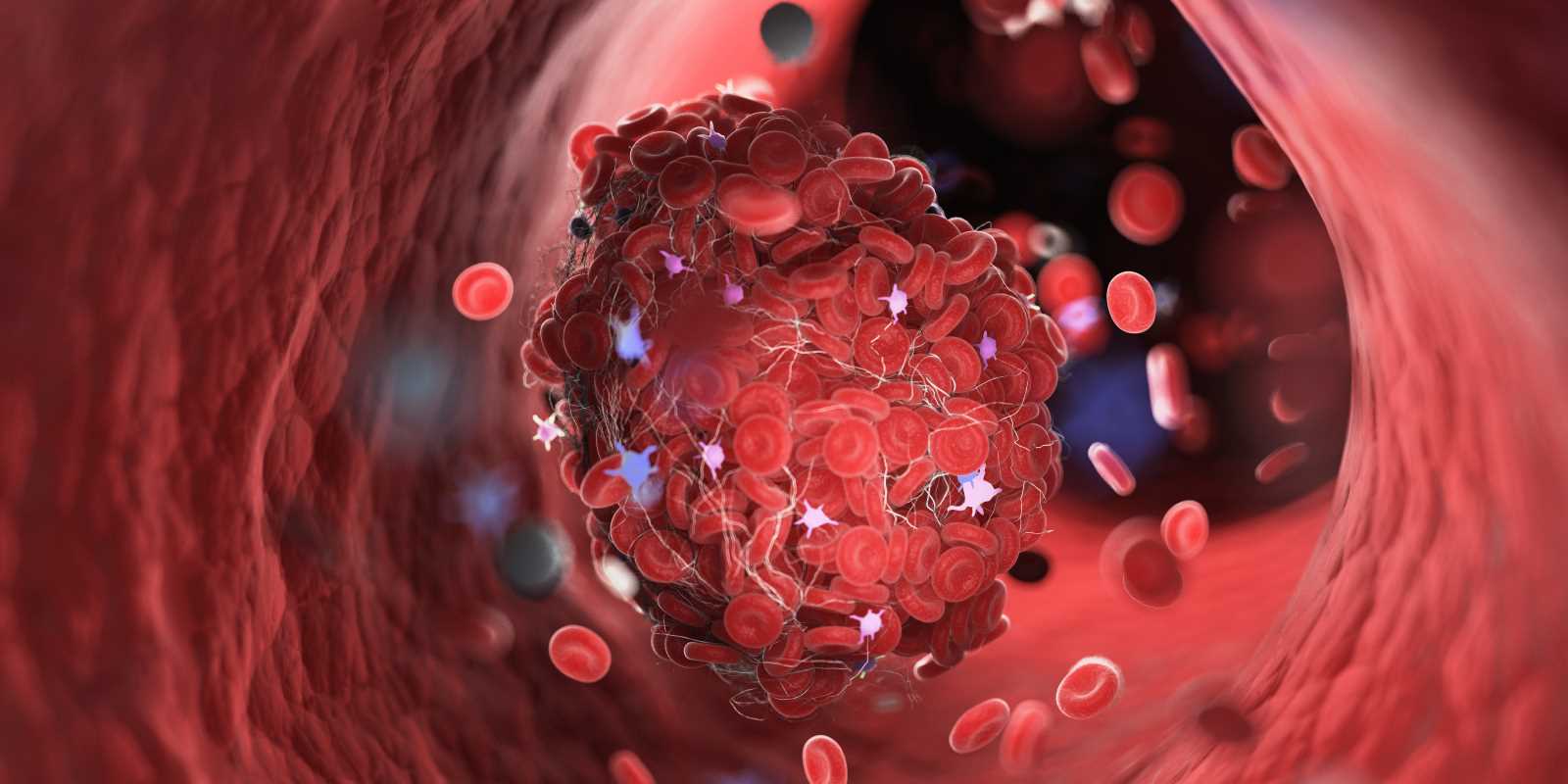
The mechanism is straightforward: when your liver produces less cholesterol, it removes more from your bloodstream to meet your body's needs. This process reduces the buildup of cholesterol plaques in your arteries, which can lead to heart attacks and strokes over time.
Research shows statins can reduce LDL cholesterol by 25-50%, depending on the specific medication and dosage. This reduction translates into meaningful cardiovascular protection for many people, particularly those with elevated risk factors.
The Compelling Benefits of Statin Therapy
Proven Cardiovascular Protection
Extensive research demonstrates that statins significantly reduce the risk of heart attacks, strokes, and cardiovascular death. Large-scale studies involving hundreds of thousands of participants show consistent benefits across different populations and age groups.
For adults over 40 with elevated cholesterol levels, statins can reduce the risk of major cardiovascular events by approximately 20-25%. This protection extends beyond just lowering cholesterol numbers—statins also reduce inflammation in blood vessels and help stabilize existing plaques, making them less likely to rupture and cause heart attacks.
Multiple Health Benefits Beyond Cholesterol
Statins offer several additional benefits that extend beyond their primary cholesterol-lowering effects:
Anti-inflammatory Properties: These medications reduce C-reactive protein levels, a marker of inflammation that contributes to heart disease progression. Lower inflammation levels benefit your entire cardiovascular system.
Plaque Stabilization: Statins help strengthen the fibrous caps covering cholesterol plaques, making them less prone to rupturing and causing blood clots.
Improved Blood Vessel Function: These medications enhance the function of the endothelium, the inner lining of blood vessels, promoting better circulation and flexibility.
Established Safety Profile
Decades of clinical use have established a well-documented safety profile for statin medications. Most people tolerate them well, and serious side effects remain relatively uncommon. The extensive real-world experience with these medications provides reassurance about their long-term safety when used appropriately.
Potential Drawbacks and Side Effects
Muscle-Related Symptoms
The most commonly reported side effect involves muscle pain, weakness, or cramping. Studies suggest this occurs in 5-10% of statin users, though the actual percentage remains debated among healthcare professionals. These symptoms typically affect the larger muscle groups in the legs, shoulders, and back.
Most muscle-related symptoms are mild and resolve when switching to a different statin or adjusting the dosage. Severe muscle breakdown (rhabdomyolysis) is extremely rare, occurring in less than 0.1% of users.
Potential Blood Sugar Effects
Statins may slightly increase blood glucose levels and the risk of developing Type 2 diabetes. This effect appears more pronounced in people already at risk for diabetes due to other factors like obesity, family history, or metabolic syndrome.
The cardiovascular benefits of statin therapy typically outweigh this diabetes risk, even for people who develop elevated blood sugar levels while taking these medications.
Liver Function Considerations
Statins can occasionally cause elevation in liver enzymes, though serious liver damage remains very rare. Healthcare providers monitor liver function through periodic blood tests, especially during the first year of treatment.
Most enzyme elevations are temporary and resolve without permanent liver damage. Discontinuing the medication typically returns liver function to normal levels.
Cognitive Concerns
Some people report memory problems or cognitive difficulties while taking statins. Research on this topic shows mixed results, with some studies suggesting minor effects while others find no significant cognitive impact.
The FDA has acknowledged these reports but notes that cognitive symptoms appear reversible when the medication is discontinued. Current evidence doesn't support avoiding statins due to cognitive concerns alone.
Who Benefits Most from Statin Therapy
High-Risk Individuals
People with multiple cardiovascular risk factors gain the greatest benefit from statin therapy. These risk factors include:
Existing Heart Disease: Individuals with a history of heart attacks, strokes, or coronary artery disease receive substantial protection from statin therapy, regardless of their current cholesterol levels.
Diabetes: Adults with Type 1 or Type 2 diabetes face elevated cardiovascular risk and typically benefit from statin therapy, especially after age 40.
Family History: Strong family histories of early heart disease indicate genetic predisposition that statins can help address.
Multiple Risk Factors: Combinations of high blood pressure, smoking, obesity, and elevated cholesterol create compound risks that statins help mitigate.
Moderate-Risk Considerations
For people with moderate cardiovascular risk, the decision becomes more individualized. Healthcare providers use risk calculators that consider age, gender, cholesterol levels, blood pressure, smoking status, and other factors to estimate 10-year cardiovascular risk.
Generally, people with a 10-year risk of 7.5% or higher may benefit from statin therapy, though this threshold continues to evolve as research advances.
Alternative Strategies for Managing Cholesterol
Dietary Approaches
Comprehensive dietary changes can significantly impact cholesterol levels without medication:
Mediterranean Diet Pattern: Emphasizing olive oil, nuts, fish, fruits, vegetables, and whole grains can reduce LDL cholesterol by 8-15%.
Soluble Fiber Sources: Oats, beans, lentils, and fruits containing soluble fiber actively lower cholesterol absorption in your digestive system.
Plant Stanols and Sterols: These compounds, found naturally in nuts and vegetable oils, block cholesterol absorption and can reduce LDL levels by 6-15%.
Exercise and Lifestyle Modifications
Regular physical activity provides multiple cardiovascular benefits:
Aerobic Exercise: Activities like brisk walking, cycling, or swimming for 150 minutes weekly can raise HDL (good) cholesterol and improve overall heart health.
Strength Training: Resistance exercises twice weekly support healthy cholesterol profiles and provide additional cardiovascular benefits.
Weight Management: Losing even modest amounts of excess weight can improve cholesterol levels and reduce cardiovascular risk.
Stress Management and Sleep
Chronic stress and poor sleep quality negatively impact cholesterol levels and cardiovascular health. Implementing stress reduction techniques and prioritizing adequate sleep support healthy cholesterol management.
Making Your Decision: Key Considerations
Personal Risk Assessment
Work with your healthcare provider to evaluate your individual cardiovascular risk profile. This assessment should consider your current health status, family history, lifestyle factors, and personal preferences about medication use.
Quality of Life Factors
Consider how potential side effects might impact your daily activities and overall quality of life. Some people prefer lifestyle modifications as a first approach, while others appreciate the proven protection that statins provide.
Long-term Commitment
Statin therapy typically requires long-term use to maintain benefits. Consider your willingness to take daily medication and undergo periodic monitoring blood tests.
Cost and Access
Evaluate insurance coverage and medication costs, as well as your access to regular healthcare monitoring. Generic statins have made these medications more affordable, but costs still vary.
Working with Your Healthcare Team
The decision about statin therapy should involve thorough discussion with your healthcare provider. Come prepared with questions about your specific risk factors, potential benefits, and concerns about side effects.
Regular follow-up appointments allow for monitoring of both benefits and potential side effects. Most people start with lower doses that can be adjusted based on response and tolerance.
Your healthcare team can also help coordinate comprehensive approaches that combine medication with lifestyle modifications for optimal cardiovascular protection.
 (Image via
(Image via.jpg)