Menopause. One minute you're perfectly comfortable, and the next you're drenched in sweat from a hot flash that seems to come from nowhere. Sound familiar? If you're wrestling with these changes, you're probably wondering whether hormone therapy could be your ticket to feeling like yourself again. The decision to try hormone therapy isn't straightforward. With so much conflicting information out there, it's easy to feel confused.
Let's explore the real benefits, potential risks, and practical considerations that can help you make an informed choice about whether hormone therapy deserves a place in your menopause management toolkit.
Understanding Hormone Therapy: The Basics
Hormone therapy replaces the estrogen and progesterone your body gradually stops producing during menopause. Think of it as giving your body a helping hand during this major transition. These hormones have been your behind-the-scenes partners for decades, influencing everything from your sleep patterns to bone strength.
There are two main types of hormone therapy to consider:
Estrogen-only therapy works well for women who've had their uterus removed. Since you no longer need progesterone to protect the uterine lining, estrogen alone can effectively manage symptoms.
Combination therapy includes both estrogen and progesterone (or progestin, the synthetic version). This approach protects women who still have their uterus from developing endometrial cancer while addressing menopausal symptoms.
The delivery methods have expanded dramatically beyond the traditional pill. You'll find patches, gels, creams, rings, and even pellets that release hormones slowly over time. This variety means you and your doctor can find an approach that fits your lifestyle and preferences.
The Compelling Benefits of Hormone Therapy
When hormone therapy works well, the relief can be life-changing. Many women discover they can finally sleep through the night without waking up soaked in sweat or spend time with friends without worrying about sudden mood swings.
Hot Flash Relief That Actually Works
Hot flashes rank as the most common reason women consider hormone therapy, and for good reason. These sudden surges of heat can strike dozens of times daily, disrupting work meetings, social gatherings, and precious sleep time. Hormone therapy reduces both the frequency and intensity of hot flashes by 80-90% in most women.
Night sweats often disappear alongside hot flashes, which means better sleep quality and more energy during the day. When you're well-rested, everything else becomes more manageable.
Mood Stability You Can Count On
The emotional ups and downs of menopause can strain relationships and make daily life feel unpredictable. Many women describe feeling like strangers in their own bodies as familiar situations trigger unexpected reactions.
Hormone therapy helps stabilize mood swings by maintaining more consistent hormone levels. While it's not a cure for depression or anxiety, many women find their emotional resilience improves significantly when their hormones are more balanced.
Protecting Your Bones for the Future
Estrogen plays a crucial role in maintaining bone density. As levels decline during menopause, your risk of osteoporosis increases substantially. This silent condition weakens bones gradually, often without symptoms until a fracture occurs.
Hormone therapy can slow bone loss and even help rebuild some bone density when started within 10 years of menopause. This protection extends throughout treatment and provides lasting benefits even after stopping therapy.
Additional Wellness Benefits
Beyond the headline benefits, hormone therapy may offer other advantages. Some women experience improved skin elasticity, better vaginal lubrication, and reduced risk of colorectal cancer. These secondary benefits can significantly impact quality of life and long-term health.
Understanding the Risks: An Honest Assessment
Every effective treatment comes with potential downsides, and hormone therapy is no exception. Understanding these risks helps you weigh them against potential benefits based on your personal health profile.
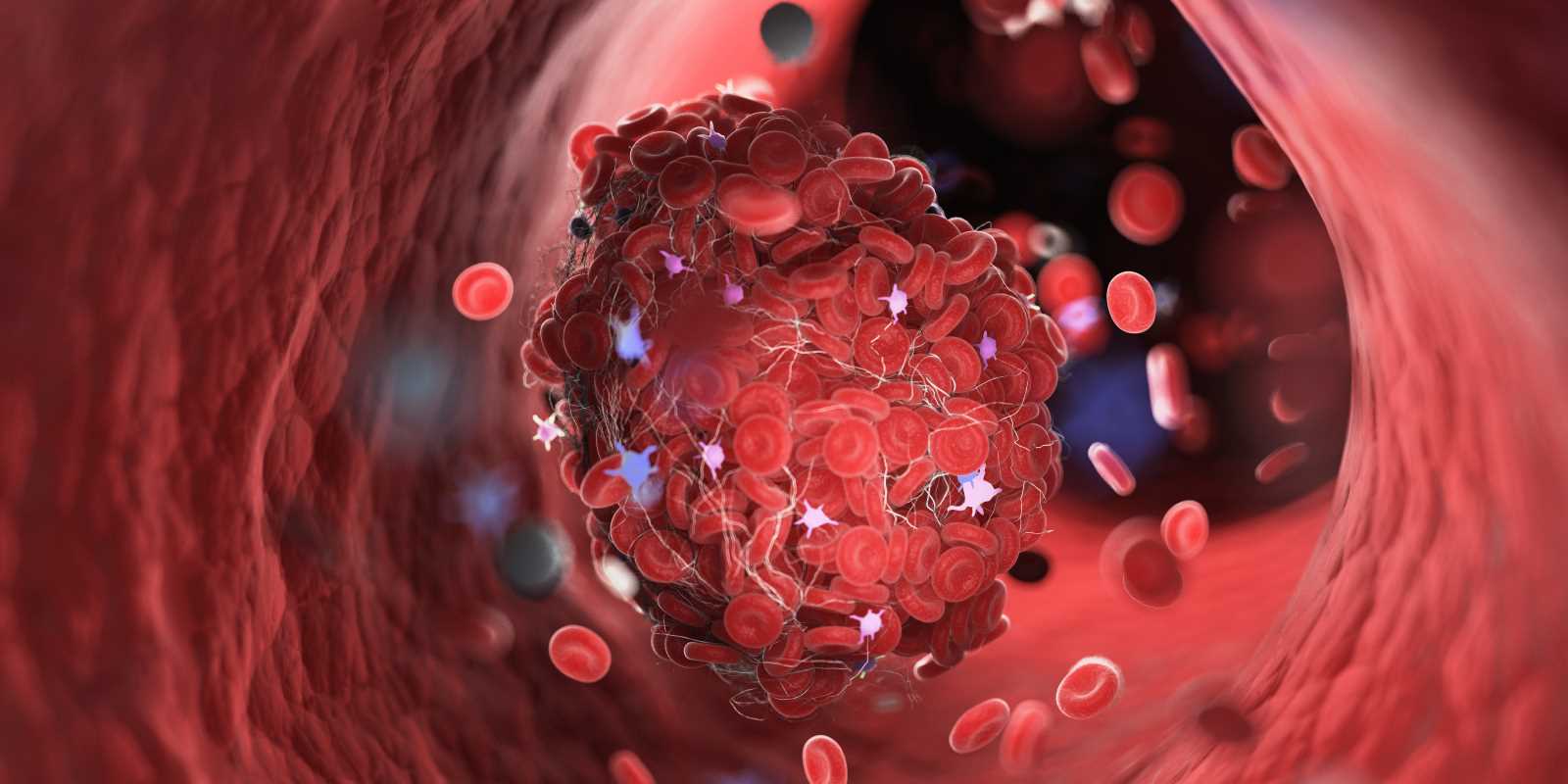
Blood Clot Considerations
Oral hormone therapy slightly increases the risk of blood clots, particularly in the legs and lungs. This risk is higher during the first year of treatment and among women with other clot risk factors like obesity or a family history of clotting disorders.
The absolute risk remains small—about 1-2 additional cases per 1,000 women per year. Transdermal options like patches and gels appear to carry lower clot risks than pills, making them preferable for some women.
Breast Cancer: The Complex Picture
The relationship between hormone therapy and breast cancer has generated intense debate and research. Large studies suggest that combination therapy may increase breast cancer risk when used for more than 5 years, while estrogen-only therapy shows little to no increased risk.
The absolute risk increase is modest—about 4 additional cases per 1,000 women using combination therapy for 10 years. Regular mammograms and breast self-exams become even more important during hormone therapy.
Stroke Risk Factors
Women over 60 who start hormone therapy face a slightly elevated stroke risk, particularly with oral preparations. This risk appears minimal for healthy women in their 50s who start therapy closer to menopause onset.
Your personal stroke risk factors, including blood pressure control and family history, influence whether this concern applies to your situation.
Who Benefits Most from Hormone Therapy?
Hormone therapy works best for specific groups of women dealing with particular challenges. Understanding whether you fit these profiles can guide your decision-making process.
Ideal candidates often include women experiencing severe hot flashes and night sweats that significantly impact daily life and sleep quality. If you're within 10 years of your last menstrual period and have no major risk factors, hormone therapy may offer excellent symptom relief.
Women who've had early menopause—whether natural or surgical—frequently benefit from hormone therapy to protect against long-term health risks like osteoporosis and heart disease. In these cases, treatment typically continues until the average age of natural menopause.
Women at higher risk for complications include those with a personal history of breast cancer, blood clots, stroke, or liver disease. Current smokers face elevated clot risks, making hormone therapy less advisable without smoking cessation.
Age plays a significant role in risk-benefit calculations. Starting hormone therapy after age 60 or more than 10 years past menopause increases risks while potentially reducing benefits.
Having the Right Conversation with Your Doctor
Discussing hormone therapy with your healthcare provider requires preparation and honesty. Come armed with specific information about your symptoms, health history, and concerns to make the most of your appointment time.
Questions That Matter
Start by describing your symptoms in detail. "How often do you experience hot flashes?" and "How severely do they impact your daily activities?" help your doctor understand the urgency of your situation. Don't minimize symptoms that truly bother you—your quality of life matters.
Ask about different hormone therapy options and delivery methods. "What are the pros and cons of patches versus pills for someone with my health profile?" opens up important discussions about personalized treatment approaches.
Explore risk factors specific to your situation. "Given my family history of heart disease, how does that influence my hormone therapy decision?" ensures your treatment plan considers your unique health picture.
Sharing Your Complete Health Story
Be thorough about your medical history, including surgeries, medications, and supplements. Your doctor needs this complete picture to identify potential interactions or contraindications.
Family health history provides crucial context. Heart disease, stroke, blood clots, and various cancers in immediate family members can influence treatment recommendations.
Lifestyle factors like smoking, alcohol consumption, exercise habits, and stress levels all impact hormone therapy decisions. Honest discussion about these topics leads to better treatment planning.
Alternative Approaches When Hormone Therapy Isn't Right
Not everyone can or wants to use hormone therapy, but that doesn't mean you're stuck suffering through menopausal symptoms. Several effective alternatives can provide significant relief.
Prescription Non-Hormonal Options
Selective serotonin reuptake inhibitors (SSRIs) like paroxetine and venlafaxine can reduce hot flash frequency by 40-60%. These medications also help with mood symptoms, making them valuable for women dealing with both physical and emotional menopausal challenges.
Gabapentin, originally developed for seizures, effectively reduces hot flashes and may improve sleep quality. Many women find this option helpful when hormones aren't suitable.
Clonidine, a blood pressure medication, can reduce hot flash frequency and intensity. While not as effective as hormones, it provides meaningful relief for many women.
Lifestyle Modifications That Work
Regular exercise, particularly cardiovascular activity and strength training, can reduce hot flash frequency and intensity while improving mood and bone health. Aim for 150 minutes of moderate activity weekly.
Stress management techniques like meditation, yoga, or deep breathing exercises help many women cope with symptoms more effectively. Chronic stress can worsen menopausal symptoms, making stress reduction particularly valuable.
Sleep hygiene improvements can dramatically impact how you feel during the day. Keep your bedroom cool, invest in moisture-wicking sleepwear, and maintain consistent sleep schedules.
Dietary adjustments may help some women. Limiting caffeine, alcohol, and spicy foods can reduce hot flash triggers, while increasing calcium and vitamin D supports bone health.
Disclaimer: The content provided on SuperHealthyTips is for informational and educational purposes only. This information is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
 (Image via
(Image via.jpg)